Vegetarians and LDL levels
In epidemiologic studies, a low serum LDL-C of less than 75 mg/dL (≈ 2 mmol/L), typically found in vegetarians and those on non-Western style diets, protects against atherosclerotic cardiovascular disease. Dietary saturated fat and cholesterol generally raise the level of LDL-C in the blood and proportionally raise the coronary risk. The related factors of obesity, metabolic syndrome, and type 2 diabetes may have only modest effects on LDL-C levels, but they increase coronary risk by increasing triglycerides and LDL particle concentration, while lowering HDL-C and causing the production of small, dense LDL particles.
• An HDL level of 50 mg/dL (≈ 1.3 mmol/L) or greater in a man or 60 mg/dL (≈ 1.6 mmol/L) in a woman is associated with a reduced risk of atherosclerosis.
• An HDL level of over 75 mg/dL (≈ 2 mmol/L) or greater in a man or woman is associated with a very low risk of atherosclerosis.
• An HDL of less than 40 mg/dL (≈ 0.8 mmol/L) in a man and less than 50 mg/dL (≈ 1 mmol/L) in a woman increases the risk of atherosclerosis.
• Low HDL levels appear as an independent risk factor for CV events when combined with high LDL levels.
- LDL Cholesterol – Primary Target of Therapy
<100 Optimal 100-129 Near Optimal/Above Optimal 130-159 Borderline High 160-189 High  190
190Very high - Total Cholesterol
<200 Desirable 200-239 Borderline High  240
240High - HDL Cholesterol
<40 Low  60
60High

LDL
The evidence that high LDL concentrations play a causal role in coronary artery disease (CAD)is quite compelling.
- Many investigators have convincing demonstrated a progressive increase in risk that correlates directly with LDL concentrations.
- Treatments that lower LDL cholesterol reduce the risk of CAD.
- Genetic studies analyzing SNPs
 show that SNPs affecting LDL cholesterol are consistently related to risk of myocardial infarction. In other words, genetic variants associated with elevated LDL levels are consistently associated with increased risk.
show that SNPs affecting LDL cholesterol are consistently related to risk of myocardial infarction. In other words, genetic variants associated with elevated LDL levels are consistently associated with increased risk. - The presence of LDL in atherosclerotic plaques provides additional evidence of its direct involvement.
Statin Drugs
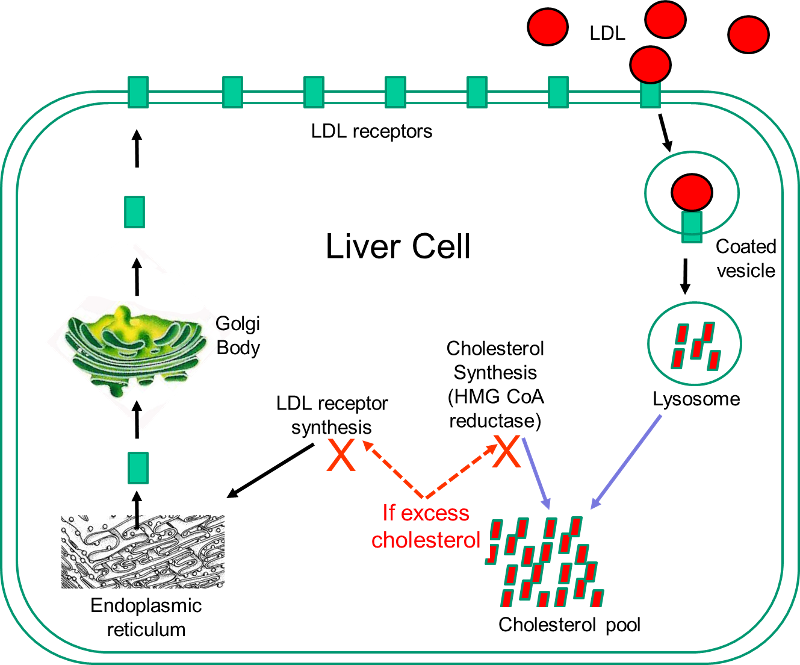 Statins are currently the most powerful cholesterol-lowering drugs available. They act by inhibiting the action of 3-hydroxy-3-methyl-glutaryl-coenzyme A (HMG-CoA) reductase, which is the rate-limiting enzyme in the sequence of steps by which cholesterol is synthesized in the liver. The liver has two sources of cholesterol: it can take up LDL particles from the blood, or it can synthesis cholesterol using HMG-CoA reductase. The diagram to the right illustrates cholesterol homeostasis in a liver cell. LDL (shown in red) can bind to LDL receptors on the surface of the liver. Binding causes the LDL to be taken up by the liver cell and digested in a lysosome. Fatty acids and amino acids in the LDL are recycled, and the cholesterol enters the cholesterol pool in the liver cell. Note that if the liver cell synthesizes cholesterol, this too will be added to the cholesterol pool. If the concentration of cholesterol in the liver cells exceeds a certain level, HMG CoA reductase is inhibited, and the synthesis of LDL receptors is also inhibited.
Statins are currently the most powerful cholesterol-lowering drugs available. They act by inhibiting the action of 3-hydroxy-3-methyl-glutaryl-coenzyme A (HMG-CoA) reductase, which is the rate-limiting enzyme in the sequence of steps by which cholesterol is synthesized in the liver. The liver has two sources of cholesterol: it can take up LDL particles from the blood, or it can synthesis cholesterol using HMG-CoA reductase. The diagram to the right illustrates cholesterol homeostasis in a liver cell. LDL (shown in red) can bind to LDL receptors on the surface of the liver. Binding causes the LDL to be taken up by the liver cell and digested in a lysosome. Fatty acids and amino acids in the LDL are recycled, and the cholesterol enters the cholesterol pool in the liver cell. Note that if the liver cell synthesizes cholesterol, this too will be added to the cholesterol pool. If the concentration of cholesterol in the liver cells exceeds a certain level, HMG CoA reductase is inhibited, and the synthesis of LDL receptors is also inhibited.
Statins act by inhibiting HMG-CoA reductase and shutting off internal cholesterol production. In this way, statins reduce cholesterol concentrations in liver cells, which causes increased production of LDL receptors and increased uptake of LDL by the liver. This ultimately results in a lowering of blood concentrations of LDL cholesterol, and this generally results in a slower progression of atherosclerotic plaques and a reduced risk of plaque rupture. However, observers occasionally report regression of atherosclerotic plaques in patient on statins.
While statins are effective in reducing LDL cholesterol levels, they can be associated with side effects.
- Muscle damage manifest as pain, tiredness, or weakness is the most common side effect and ranges from mild discomfort to difficulty in climbing stairs or walking. Statins very rarely cause severe, life-threatening rhabdomyolysis
 which can result in severe muscle pain, liver damage, kidney failure, and death.
which can result in severe muscle pain, liver damage, kidney failure, and death. - Liver damage: Statins can also damage liver cells, resulting in elevated levels of liver enzymes in blood. Liver enzyme levels should be monitored when statins are first started.
- Digestive problems: Some people experience nausea, gas, diarrhea or constipation.
- Rash or flushing
- Increased blood sugar or type 2 diabetes is occasionally seen in patients on statins.
Because of their effectiveness in reducing CAD in patients at high risk, some advocated expanding the use of statins to people who did not necessarily have elevated cholesterol levels. A number of large, well-done clinical trials have demonstrated that statins can reduce the risk of CAD in low-risk individuals, but most experts caution against this because of the cost and the risk of side effects.