Understanding PML and the JC Virus in Multiple Sclerosis
Before AIDS epidemic, PML was considered a rare complication of the middle-aged and elderly patients with lymphoproliferative diseases and incidence of PML in pre-AIDS era was considerably low (0.07%) [12]. It is now a commonly encountered disease of the CNS in patients of a variety of different age groups with AIDS and ~5% of HIV patients develop PML. It is now defined as an AIDS-associated illness. In addition, recent studies indicate that the highly active retroviral therapies (HAART) against HIV infections considerably reduced the virulent behavior of HIV virus, however, the same does not hold for JCV infections. In other words, the incidence of PML did not significantly change between the pre-HAART and post-HAART era [13]. More interestingly, PML has also recently been described in patients with autoimmune diseases such as multiple sclerosis and Crohn’s disease, who were treated with specific monoclonal antibodies. These antibodies (natalizumab and efalizuma) target several surface molecules (α-integrin) on B and T cells and prevent their entry into brain, skin and gut. Rituximab, another monoclonal antibody, targets the CD20 surface molecule on B cells and causes their depletion through complement-mediated cytolysis.
PML stands for progressive multifocal leukoencephalopathy- ok lets just stop right there and breakdown that mouthful…
Progressive- steadily getting worse
Multifocal- in many areas
Leuko- white (in this case referring to white matter in the brain)
Encephalopathy- disorder or disease of the brain
So before even reading anything else you already know that this is a disease that afflicts multiple areas of white matter in the brain, and that it gets worse over time. But what causes it?
PML is in a category called “opportunistic infections”. These are infections that generally pose no threat to a person with a normal immune system, but love to rear their ugly heads in people with weakened immune systems. They are most frequently seen in chemotherapy patients or people with HIV because they are severely immunocompromised. Although it is much rarer, they can also occur in people with MS who are on drugs that weaken their immune systems. You may already know that Tysabri poses the greatest risk for developing PML. However, PML developed in one person taking Gilenya, and one person taking Tecfidera recently died of complications from a PML infection.
The JC virus (John Cunningham virus) is the infection that leads to PML. This virus behaves much like other common viral infections such as herpes and the chicken pox. When you get the chicken pox the virus never leaves your body, and later in life it may flare up again and cause a condition called shingles. Similarly, people who have been infected with herpes always have the virus lurking in their nervous systems. During times of stress it will become active and an outbreak of sores will occur, but unless an active outbreak is occurring there are no outward signs of the virus. The JC virus is fairly common, and is passed easily from person to person. However, since it’s an opportunistic infection healthy people never have any complications from it. When you introduce medications that weaken the immune system, like Tysabri does, your body no longer fights off viruses the way it used to. This gives the dormant JC virus the chance to become active. Once it is active there is a chance that it can cross through the blood-brain-barrier and cause PML. This causes severe damage to the white matter of the brain, and can even lead to death.
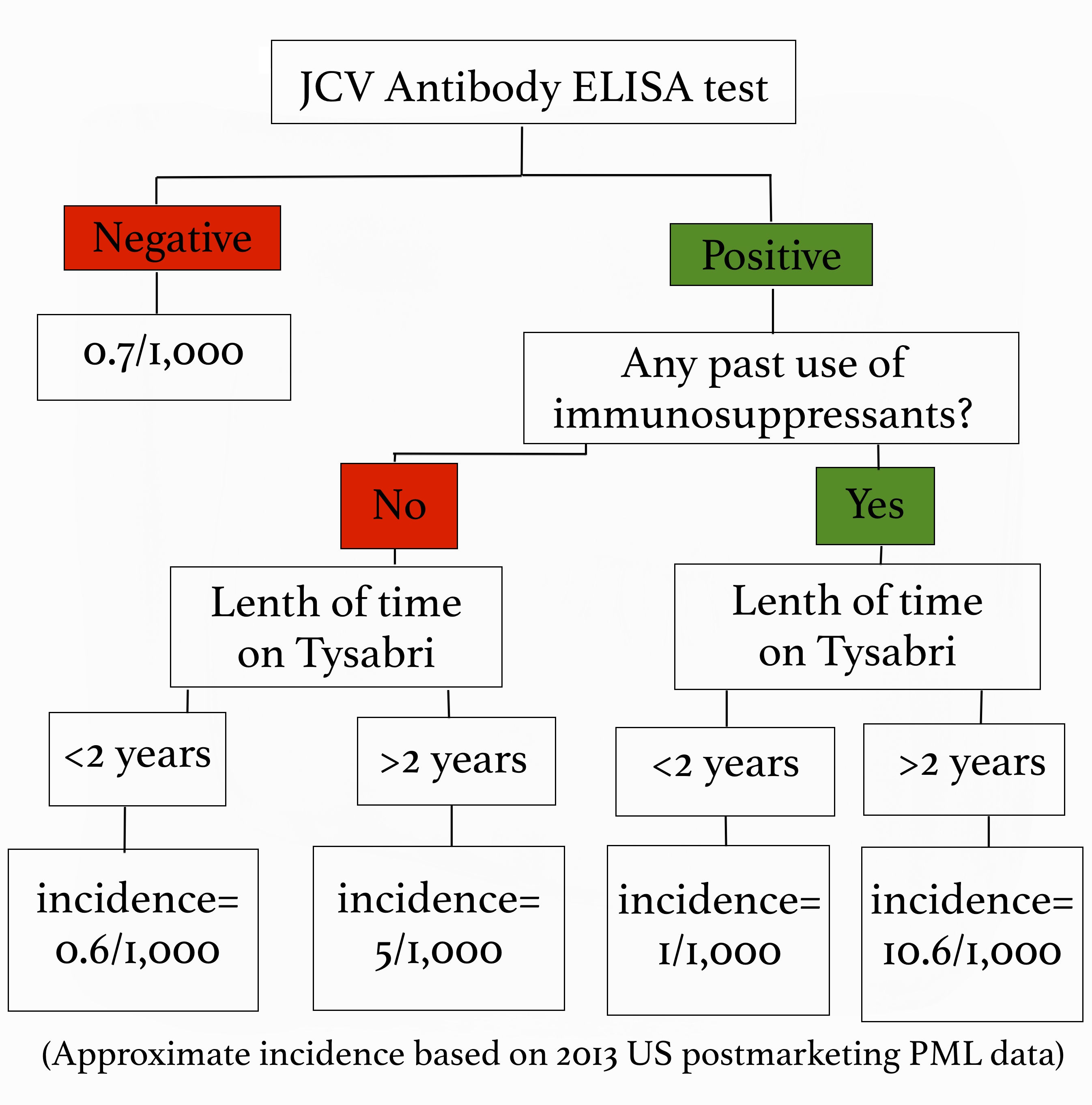
All of that information is fairly terrifying right? Well, here’s some good news! We can easily test to see if you have been exposed to the JC virus, which tells us if you are at risk for developing PML. A blood test called the JCV Antibody ELISA test is routinely done on anyone thinking about going on Tysabri. If you test negative, meaning you don’t carry the JC virus, we continue to test for it every 6 months while you are taking Tysabri because you can be exposed to the virus at any time. If you do test positive we also get an index value, which gives us even more information about how likely you are to get PML. A low index value indicates a very low risk, and a higher number indicates a greater risk. All that being said, PML is by no means a common side effect. However, when it does happen it is very serious, so we as providers aren’t willing to take any chances! During the first year of taking Tysabri your risk is very low, but it increases after two years. Additionally, being treated with immunosuppressants in the past puts you at a higher risk for developing PML. We look at all of these risk factors, and use that information to decide whether Tysabri is safe for you or not. The benefit of Tysabri is that it lowers relapse rates by 81%, and disability progression by 64% so we have to weigh its effectiveness against the relative risk of contracting PML, which I’ve summarized for you below:
Because PML attack the myelin, just like MS does, the symptoms should sound familiar. They include confusion, difficulty talking, weakness, memory loss, and loss of balance and coordination. If PML is suspected a MRI of the brain will be done, and a lumbar puncture can confirm the diagnosis. PML is treated in the hospital, and the goal of therapy is to remove all traces of the virus from your body.1-6
Picking medications is a very personal decision, and should be discusses in detail with your neurologist. It is imperative to weigh the risks versus benefits very carefully, and to understand the medications and their side effects. Being well informed is the first step to being your own best advocate!
Diagnosis
Although PML lesions, caused by both lytic infection of oligodendrocytes and neuronal loss, can be detected by magnetic resonance imaging (MRI) system [33], some other CNS related viral infections may make this diagnosis difficult. Therefore, detection of JCV in the brain samples of PML patients in large numbers would be strong evidence for the full diagnosis of the disease. There are a number of techniques for the identification of the virus as the causative agent of PML, including immunocytochemistry and nucleic acid methods. Antibodies against JCV were employed earlier; however, the specificity of this method was always in question due to cross-reactivity with other viral proteins. Nucleic acid methods, such as in situ hybridization of JCV DNA were successfully performed on tissue samples obtained from various PML patients [34]. However, the polymerase chain reaction (PCR) has been proven to be the most reliable method for detecting JCV DNA in PML cases. PCR can easily be used to test cerebrospinal fluid (CSF) for infectious JCV. In a recent study, it has been shown that as low as 10 copies of viral DNA in CSF can be detected using quantitative PCR technology [35].To support this finding, in another recent study, 168 suspected PML cases over 10 years have been reviewed retrospectively and it turned out that majority of the samples that are diagnosed as JCV positive using PCR come from HIV positive patients [36], which highlights the importance of HIV infection in JCV reactivation.